What is intervertebral disc degeneration?
Back pain is a prevalent issue among adults, with certain research indicating that chronic low back pain affects as many as 23% of the global adult population. One of the most common causes of lower back pain is intervertebral disc degeneration (IDD). Intervertebral joint degeneration refers to the progressive deterioration or wear-and-tear of the joints situated between adjacent vertebrae in the spine. These discs serve as cushions between two vertebrae in the spinal column, offering stability while enabling movement between the vertebrae. Over time, various factors such as aging, genetic predisposition, repetitive stress, or injury can contribute to the degeneration of these discs. As intervertebral joint degeneration advances, the discs may lose their ability to absorb shock and distribute forces effectively. This can result in a range of spinal issues, including reduced mobility, stiffness, and chronic low back pain. Additionally, as the intervertebral discs degenerate, they can progress to other spinal conditions such as disc herniation or facet joint arthritis, further affecting an individual’s overall spine health and quality of life.
Pathogenesis
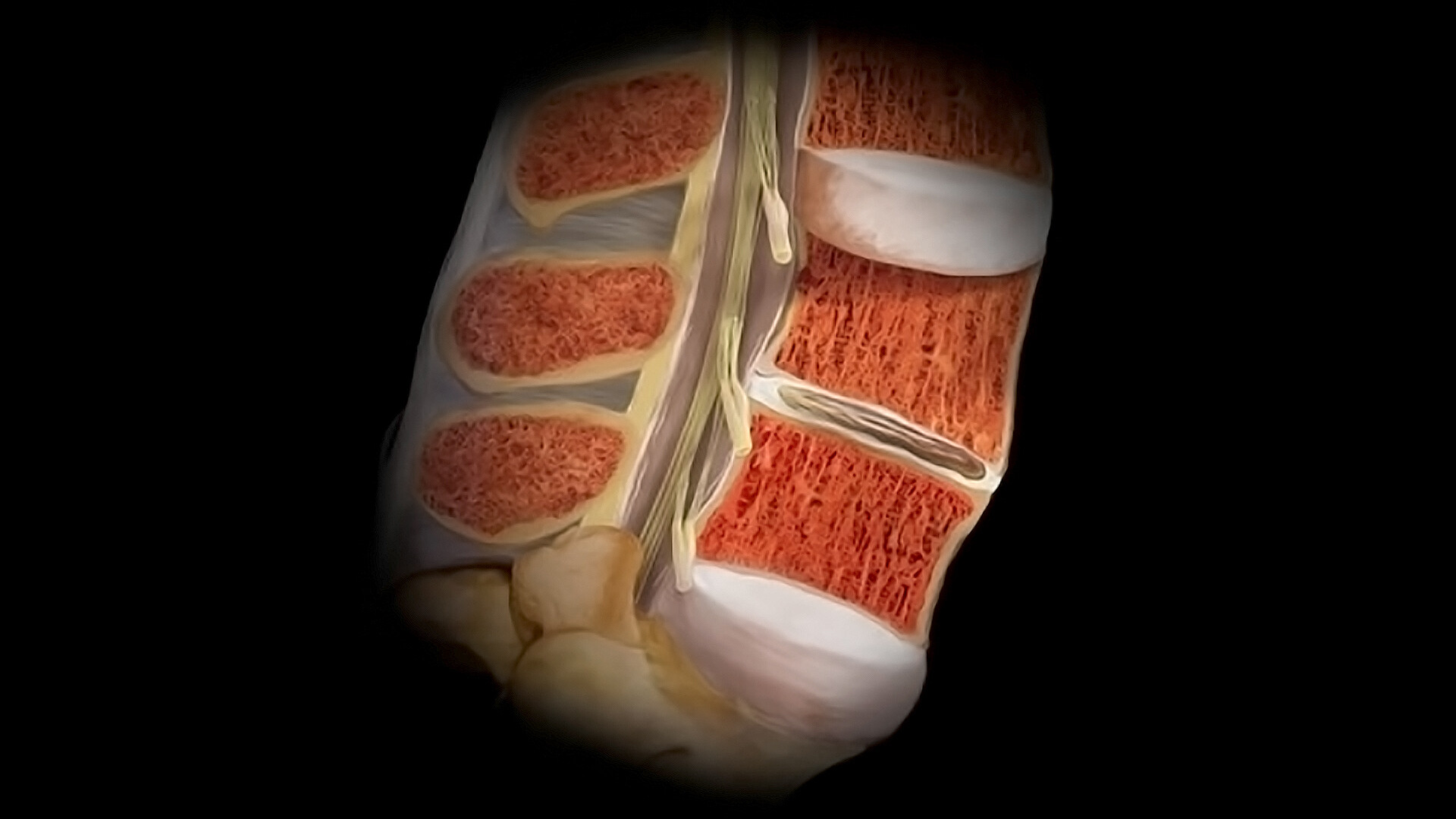
Understanding the intervertebral disc’s (IVD) structure is crucial in the context of IDD. The IVD consists of the nucleus pulposus (NP), the annulus fibrosus (AF), and the cartilaginous endplates (CEPs). The NP serves as its core, comprising various cell types and a matrix rich in proteoglycans and collagen type II, allowing it to resist pressure and maintain hydration.
The AF surrounds the NP, mainly composed of collagen type I. The inner AF, adjacent to the NP, contains more collagen type II and proteoglycans, while the outer AF is dominated by collagen type I. The CEPs, on the outer side of the IVD, play a critical role
in nutrient supply through a diffusion mechanism.
IDD involves structural and biochemical changes over time, including CEP calcification, notochordal cell loss, and disrupted nutrient diffusion. This leads to an acidic environment due to increased lactic acid, causing cell apoptosis. MMPs’ increased activity accelerates the degenerative process.
Inflammatory mediators like interleukins and TNF-α worsen IDD by disrupting collagen and proteoglycan synthesis while increasing MMP activity, triggering pain sensations as nerve fibers penetrate deeper into the degenerating IVD. This interaction contributes to IDD’s painful symptoms.
The IVD’s microenvironment undergoes significant alterations during IDD, making it challenging for the regeneration process to occur naturally. The current treatment approaches, whether conservative or surgical, primarily focus on pain relief and muscular stabilization but have not demonstrated optimal results in restoring the degenerated IVD to its former state. These limitations have spurred research into innovative solutions for IDD reversal and tissue regeneration, with a growing interest in the therapeutic potential of stem cells, particularly adipose-derived stem cells (ASCs), bone marrow aspirate concentrate (BMAC), and Bone Marrow Mesenchymal Stromal
Cells (BM-MSCs).
Adipose-Derived Stem Cells (ASCs)
ASCs hold great promise in regenerative medicine due to their versatility, capable of differentiating into various cell types and functioning as immunomodulators to aid tissue healing. They offer advantages like easy procurement, minimal donor site morbidity, rapid proliferation, and strong differentiation capabilities.
Ongoing research focuses on optimizing ASC preparation and exploring applications in disorders like intervertebral disc degeneration (IDD). ASCs aid IDD regeneration by differentiating into relevant cell types and releasing healing-promoting cytokines and growth factors. Factors like SDF-1 chemokines and VEGF influence angiogenesis, driving ASC migration to damaged areas. Animal studies show promise, with injected ASCs mitigating disc height loss and restoring disc signal intensity.
Clinical trials, however, yield mixed results. While animal experiments demonstrate potential IVD regeneration with stem cell injection, recent clinical trials report limited symptom improvement in discogenic low back pain patients. Smaller case studies suggest stem cell therapy may relieve pain and enhance IVD function, but comprehensive evaluations require larger multicenter clinical trials with standardized protocols.
Bone Marrow Aspirate Concentrate (BMAC) and Culture-Expanded Bone Marrow Mesenchymal Stromal Cells (BM-MSCs)
BMAC and BM-MSCs, like ASCs, are of mesenchymal origin; however, these stem cells are derived from bone marrow instead of adipose tissue. In the past, mesenchymal stem cells (MSCs) were typically sourced from bone marrow, resulting in what’s known as bone marrow-derived MSCs. This aspirate can be employed in its original form, cultured to increase cell numbers (as in BM-MSCs),or subjected to minimal adjustments to form bone marrow aspirate concentrate using centrifugation techniques (as in BMAC).
New research
on BMAC and BM-MSC intradiscal injections for discogenic pain suggest promising outcomes. Injections of bone marrow aspirate concentrate(BMAC) or culture-expanded bone marrow mesenchymal stem cells (BM-MSCs),whether autologous or allogeneic, generally lead to improved pain intensity and physical function in patients compared to baseline or control groups. Some MRI evidence indicates better disc characteristics, although this varies between studies. Notably, these benefits persist for up to six years, with lumbar injections showing reduced opioid use and a majority of patients avoiding surgery. The mechanism behind pain relief appears to be rooted in the immunomodulatory properties of BMAC and BM-MSCs, as they release factors that reduce inflammation.
Umbilical Cord Stem Cells & Exosomes
Exosomes are tiny packages released by cells, carrying proteins, genetic materials, and fats. They help cells communicate with each other and can be found in body fluids like blood, urine, and breast milk. Exosomes have important roles in medical treatments, diagnosis, and promoting healing. They can reduce inflammation, stress, improve blood flow, and slow down the body’s natural wear and tear. Due to their strong anti-inflammatory properties, they are an excellent option for epidural injections around the disc. Exosomes do not contain cells; they are cell-free. This is crucial, especially when injecting them into discs ,which have low oxygen levels where regular stem cells might not survive. We use potent stem cells from umbilical cords, which are more effective than those from bone marrow. These cells are injected into worn-out facet joints in the spine to promote healing.
Eterna Disc Procedure
Based on our analysis of the current scientific evidence, we offer a unique complex spine procedure.
This is a patient who had a large disc herniation with severe nerve pain. Instead of undergoing surgery, he had a regenerative medicine procedure that healed his disc herniation. The arrow indicates the large disc material in the epidural space, which reabsorbs about 4-6 months after the procedure.
Our multi-modal procedure involves using Umbilical cord stem cells, Platelet-rich plasma (PRP)and exosomes. This process includes PRP for increasing ligament stability, stem cells into degenerated joints, and exosomes injected into the epidural space & disc.
This procedure can be applied to various body parts, including the knee, hip, shoulder, hand, wrist, foot, ankle, elbow, and spine. Spine treatments involve an additional step with antibiotics to reduce infection risk and an epidural containing exosomes.
Recovery time varies but generally involves a gradual return to normal activities over weeks to months, with the best results observed at 1-2 years after the procedure.
Post-procedure, patients may experience joint soreness for a few days, with pain medication available. They are encouraged to keep the joint still for a brief period after the procedure and limit activity on the first day. Specific braces or boots may be recommended.
Patients often notice some improvement in the first month, with pain gradually decreasing overtime. Most can resume light activities within a week, gradually increasing their exercise routine over the following weeks to months. Continued healing is observed over several months, with the best results typically seen at 1-2 years post-procedure. Results vary depending on the patient’s condition, age, and overall health.
Our proprietary stem cell processing enhances mesenchymal stem cells, resulting in a more effective product compared to standard stem cell methods. Additionally, our exosomes are specialized form that provides faster and more intense release of healing factors to promote better tissue healing. Exosomes contain 10 times more growth factors and anti-inflammatory cytokines as compared to platelet-rich plasma or platelet lysate.